A HIPAA breach can cripple your medical practice
Over the last few months we have discussed HIPAA in very general terms. I have tried to impart some of the basics of its security and privacy obligations upon each of you, while ignoring the rest of the Act.
Certainly, it is a massive undertaking to fully grasp all of HIPAAs ins-and-outs, and I will not ever try to bore you with the entire 5 sections of HIPAA. So if you need to know about Insurance Portability, Tax Matters, Group Plans, or Revenue Offsets, please feel free to read the other four Titles.
Now that we have discussed what information is subject to HIPAA and who is responsible to keep and control electronic protected health information (ePHI), it’s a good time to learn what I like to call the “so what?” of HIPAA. As I travel, meet, speak with, and interact with doctors, I am often presented with the “so what?” response.
Many doctors have told me: “Steve I understand that HIPAA exists, but we have always done it this way. I think we are compliant. Or we don’t know how to fully comply.” And almost all those conversations end with “so what if we are not compliant, no one will even look at my little office to audit us.”
So, I realized that I needed to do a little more in this blog. Let’s discuss what a breach is, what you have to do if you are in breach and finally the “so what?”, namely what are the fines?
Let’s first learn what a “breach” is and is not. A breach can be defined as the acquisition, access, use, or disclosure of protected health information in a manner not permitted, which compromises the security or privacy of the protected health information.
This means that if protected health information is in the possession of the wrong person and they can read it, a breach exists. If you give Jan Smith’s records to Jane Smith, there is a breach. Or if you fax medical records to (702) 555-1234, but the patient’s number was (712) 555-1234, you have a breach.
It’s these little mistakes that plague offices at times. Most certainly, if your patient charts are on your laptop and it’s stolen, that’s a breach. Should your server be accessed due to a hacking incident, or if you email a patient’s records to Kinkos as opposed to Dr. Kinko (the physician you intended to refer your patient to), you have a breach event.
Simply put, records must be seen only by those authorized to see them, and Covered Entities (CE) and Business Associates (BA) in possession of the records hold the responsibility to ensure no breaches take place.
“But what if my PHI is encrypted?” you ask. If the PHI is encrypted when the breach took place, you are probably covered. The unauthorized use or disclosure of PHI is presumed to be a breach, unless there is a low probability that the information was compromised.
So when the PHI ends up in the wrong hands, but all they see is 0s and 1s due to your encryption, you may be protected. If you realize an email went to joesmith@mail.org as opposed to josmith@mail.org, but the email was sent with encryption, you are probably ok not reporting a breach.
However, a breach notification is necessary in all situations except those in which the CE demonstrates through a risk assessment that there is a low probability that the PHI has been compromised. We will discuss what a “risk assessment” is in the next blog.
But today’s blog is addressing a breach. So, assuming a reportable breach took place, now what? Once a CE or BA is made aware of a possible breach, they must report the breach to the Department of Health & Human Services.
The report must be made without “unreasonable delay”. While it is not 100% certain what constitutes an “unreasonable delay”, 60 days appears to be the outer limit for reporting, and waiting until the 60th day could be unreasonable as well.
Some state laws provide stricter reporting rules such as California’s mandate that you have 5 days to report a breach. We will discuss the notice details in a later blog
And now the “So what?” Here are the federal breach penalties. But please take note that some states allow separate penalties. Additionally, some states allow private causes of action against the CE by the harmed patients. So these charts present only the tip of the iceberg in some cases.
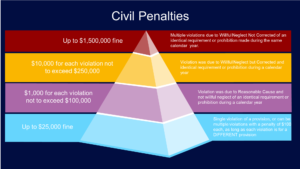
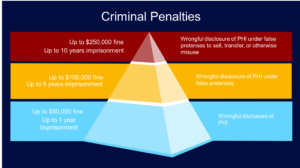
Looking through the charts it is easy to see the risks you’re taking by not making sure your office is HIPAA compliant. In 2016, the Office for Civil Rights (OCR) collected over $20 million in fines, and in 2017 they have already disclosed over $17 million in fines collected.
Finally, don’t think that just because you are only an employee for a company, that you are immune from these fines and prison sentences. If an executive is aware of a violation, delegating the responsibility to someone else (the company’s “Security Officer”, perhaps) DOES NOT protect the executive from a personal penalty.
So now that you know what the ramifications are for a HIPAA breach, it is crucial that you take the necessary steps to ensure you don’t end up as one of OCR’s statistics.
Take the painful (but important) measures to be compliant now to save yourself a lot of stress, heartache, and money in the future. Otherwise the question you’ll be asking isn’t “so what?” but rather “does anyone know a good attorney?”